A Hand-Held Ultrasound Device for the Assessment of Peripheral Nerves in Leprosy
Stephen W. Wheat, Barbara Stryjewska, and Michael S. Cartwright
From the Department of Neurology - Guest Lecturer, Baylor College of Medicine, Houston, TX, 77030 (SWW); National Hansen's Disease Program, Baton Rouge, LA, 70803 (BS); and Department of Neurology, Wake Forest School of Medicine, Winston-Salem, NC, 27157 (MSC)
ABSTRACT
BACKGROUND AND PURPOSE: Mycobacterium leprae complex affects peripheral nerves, causing nerve enlargement. This proof-of-concept pilot study was conducted to determine if a small hand-held ultrasound device can accurately identify nerve involvement in individuals with leprosy.
METHODS: Peripheral nerve ultrasound was conducted of the bilateral median (wrist, forearm, elbow, and mid-humerus), ulnar (wrist, forearm, elbow, 4 cm proximal to the elbow, and mid-humerus), C5 root, and greater auricular nerves with a standard ultrasound device (15 Mhz) and a hand-held ultrasound device (5 MHz). Nerve cross-sectional areas were compared using the two devices.
RESULTS: Eight individuals with leprosy were examined. Strong correlation was found between the standard and hand-held ultrasound devices (r = .76, P < .001). A certain amount of variability between ultrasound devices may occur for multiple reasons.
CONCLUSION: A hand-held ultrasound device can readily identify nerve enlargement in individuals with leprosy. This type of device may assist in the diagnosis of leprosy in areas with limited healthcare resources because of the portability and low-cost nature of such devices.
Keywords: Ultrasound, leprosy, portable, ulnar nerve, greater auricular nerve.
Acceptance: Received August 13, 2020. Accepted for publication September 19, 2020.
Correspondence: Address correspondence to Stephen W. Wheat, Wheat Medical Center, Natchitoches, LA 71457. E-mail: stephen@mandloffice.com.
Acknowledgments and Disclosures: Drs. Wheat, Stryjewska, and Cartwright have no disclosures and no conflicts of interest. We want to express tremendous appreciation for discussions with Dr. James Killian, Department of Neurology, Baylor College of Medicine in Houston, Texas.
J Neuroimaging 2020;00:1.
DOI: 10.1111/jon.12797
Introduction
Hansen’s disease (leprosy) is a rare infectious disease, but there are still 250,000 new cases worldwide and 200 new cases in the United States annually.[1,2] It is suspected that there are greater than 4 million individuals with leprosy undiagnosed globally at any given time.[3] It is caused by Mycobacterium leprae and Mycobacterium lepromatosis, which together are termed Mycobacterium leprae complex.[4] Leprosy affects the peripheral nerves and causes a polyneuropathy. It is effectively treated with multiple-drug therapy, but because it is common in areas with fewer healthcare resources, early identification of leprosy can be a limiting factor in its treatment. Previous studies have examined the utility of peripheral nerve ultrasound for the identification of polyneuropathy secondary to leprosy, and these studies demonstrate that those with leprosy have significant nerve enlargement (along with increased nerve vascularity).[9] We, therefore, designed this proof-of-concept pilot study to determine if a small, hand-held ultrasound device could identify nerve enlargement in those with leprosy, as this may improve diagnostic capabilities in areas of the world with limited resources because of the portability and inexpensive nature of such ultrasound devices.
Methods
Individuals with leprosy were recruited from the National Hansen’s Disease Program in Baton Rouge, LA. Institutional review board approval was obtained prior to the start of the study and all individuals provided written informed consent. Participant demographic data were obtained. One ultrasonographer (SWW) scanned the nerves of all participants using both a standard device (GE Logiq E, 15 MHz transducer, GE Healthcare, Chicago, IL) and a hand-held device (Butterfly iQ, 5 MHz transducer, Guilford, CT). The following nerves were scanned bilaterally: median at the wrist, forearm, elbow, and mid-humerus; ulnar at the wrist, forearm, elbow, 4 cm proximal to the elbow, and the mid humerus; C5 cervical root; and greater auricular nerves.13 These scanning locations were chosen because of previous ultrasound studies for leprosy and chronic inflammatory demyelinating polyneuropathy.[7,9,10-12] Cross-sectional areas were measured using the trace function on both devices, with the ultrasound positioned perpendicular to the nerve of interest and tracing just inside the hyperechoic epineurium. Each patient was scanned for a total of 30 minutes continuously. Both the Butterfly iQ (hand-held) and GE Logiq (standard) ultrasound devices required 15 minutes each of the 30 minutes total scan time.
Discreet variables were assessed as percentages and continuous variables as means and standard deviations. The mean cross-sectional areas were calculated for each nerve site, combining the right and left sides. A Pearson product-moment correlation coefficient was calculated comparing the measurements obtained with the standard and the hand-held devices. In addition, a Pearson product-moment correlation was calculated only using the three sites of most prominent enlargement (ulnar at 4 cm above elbow, ulnar at mid-humerus, and greater auricular nerve). Both left and right sided measurements were included in these analyses as it was thought this did not violate the assumption of statistical independence, because leprosy affects nerve in a patchy pattern and does not necessarily affect extremities symmetrically.
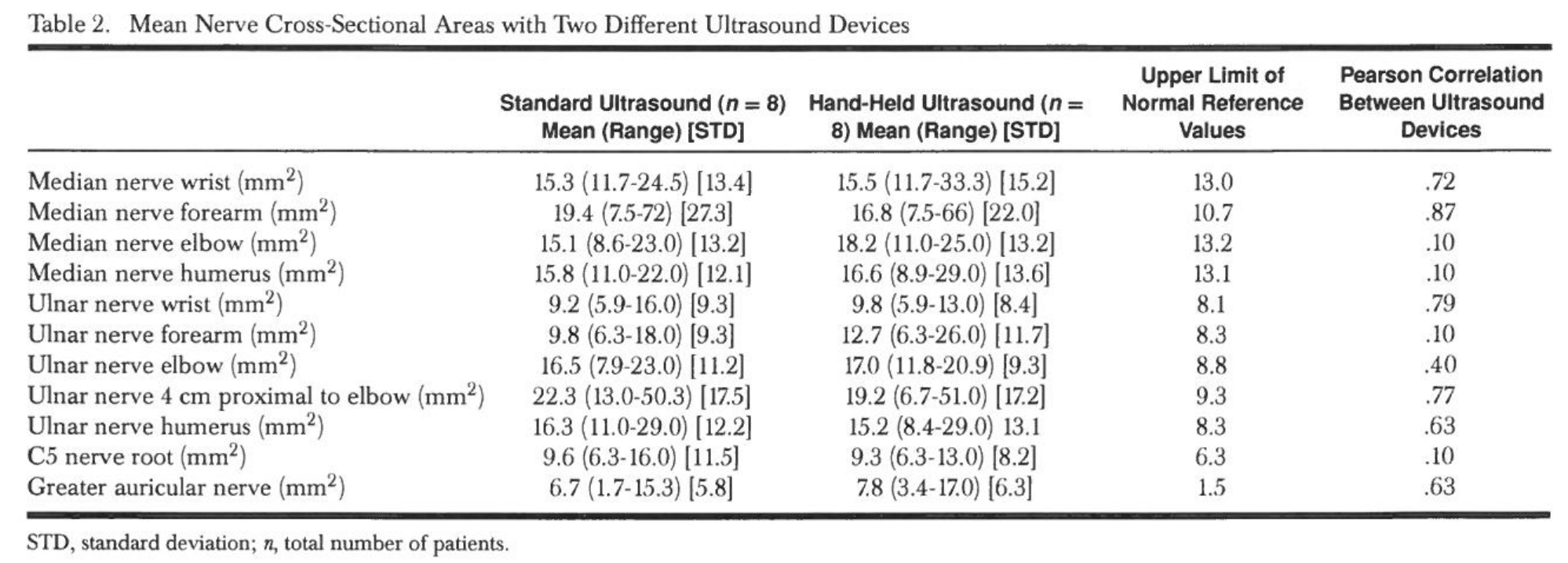
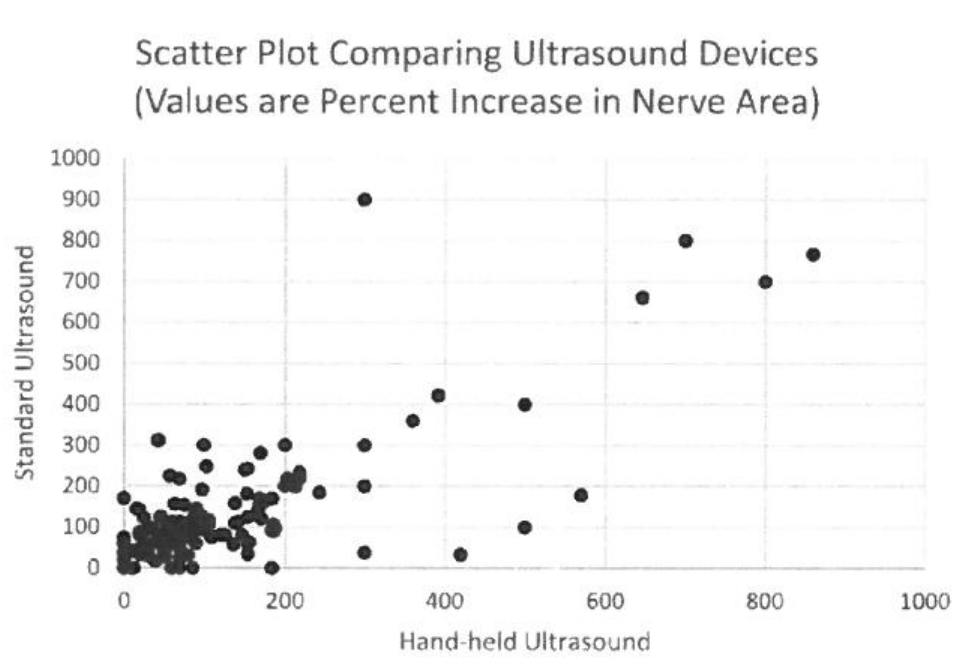
Fig 1. Percent increase in nerve cross-sectional area over the upper limit of normal of reference values are compared between standard and hand-held ultrasound devices.
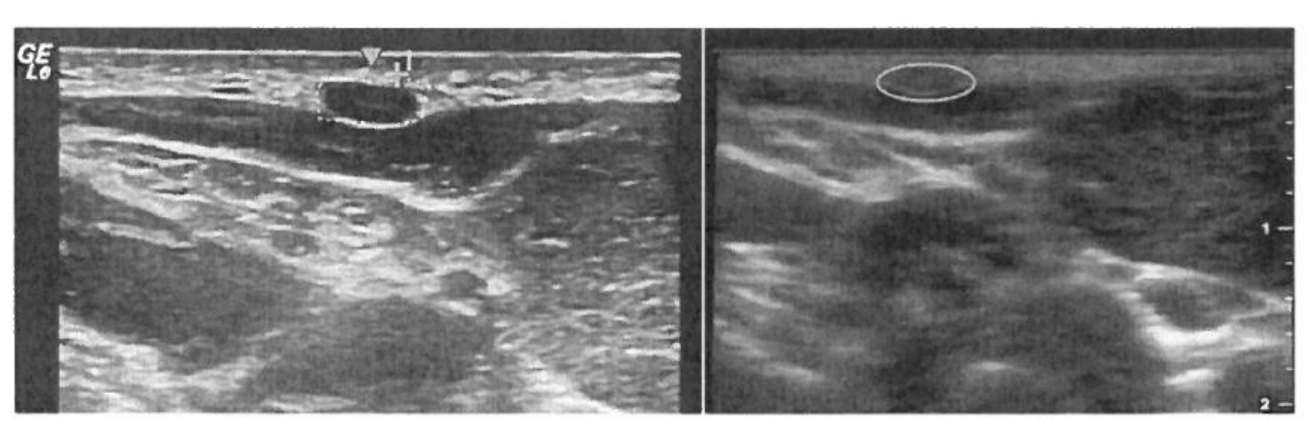
Fig 2. These images are of the left greater auricular nerve. The image with GE in the upper left corner is from the standard ultrasound device, and the other image is from the hand-held ultrasound device. The nerve is circled in both images, and it measured 9 mm2.
Results
Eight individuals with leprosy were studied. Their demographics are included in Table 1. The mean cross-sectional area values are reported in Table 2. Based on reference values,[5-7] the nerves with the greatest enlargement were the ulnar 4 cm proximal to the elbow (230% of normal), the ulnar at the midhumerus (160% of normal), and the greater auricular nerve (390% of normal). Using all sites in all individuals, the Pearson product-moment correlation was .76 (P< .001) between the cross-sectional areas measured with the standard and the handheld ultrasound devices (Fig 1), and correlations for individual sites are included in Table 2. When only the three nerves with the greatest enlargement were assessed, the Pearson product-moment correlation was .73 (P< .001) between the two devices. Figure 2 shows a representative nerve image with each device.
Discussion
This proof-of-concept pilot study demonstrated similar nerve cross-sectional areas using a standard and a small, hand-held ultrasound device in individuals with leprosy. This indicates that hand-held ultrasound device could be used to assess for nerve enlargement in individuals with suspected leprosy in areas of the world with limited healthcare resources. Hand-held ultrasound devices are highly portable, inexpensive (typically less than $3,000), and some plug into smartphones or tablets and allow teleguidance from a remote location.[8]
Nerve involvement occurs early in the course of leprosy, and it is a major cause of morbidity from the disease. It is, therefore, critical to assess for nerve involvement in individuals with suspected leprosy. Several studies of nerve ultrasound have been conducted, showing that nerve enlargement is common, as is increased vascularity (detected by Doppler imaging).9,10 It is postulated that superficial nerves are more commonly affected, perhaps because they have a lower temperature environment. Similar to previous studies, we noted the greatest nerve enlargement in the ulnar (4 cm proximal to elbow and mid-humerus) and greater auricular nerves.[9, 11]
Our study is limited by a small sample size and a lack of controls (prohibiting calculations of sensitivity and specificity). Some nerve sites had much higher correlations between the ultrasound devices than other sites, which is likely secondary to limited sample size at each site. Despite these limitations, it is clear that hand-held ultrasound devices can readily identify nerve enlargement, so the use of these types of devices should be considered for further investigations of individuals with suspected leprosy in areas with limited healthcare resources.
References
1. Rodrigues LC, Lockwood DN. Leprosy now: epidemiology, progress, challenges, and research gaps. Lancet Infect Dis 2011;11:464-70.
2, National Hansen’s Disease Program [Internet]. Available from: https://www.hrsa.gov/hansens-disease/index.html. Accessed May 30, 2020.
3. Blok DJ, De Vlas SJ, Richardus JH. Global elimination of leprosy by 2020: are we on track? Parasit Vectors 2015;8:548.
4. Singh P, Benjak A, Schuenemann VJ, et al. Insight into the evolution and origin of leprosy bacilli from the genome sequence of Mycobacterium lepromatosis. Proc Natl Acad Sci U S A 20153112:4459-64.
5. Cartwright MS, Shin HW, Passmore LV, et al. Ultrasonographic reference values for assessing the normal median nerve in adults. J Neuroimaging 2009; 19:47-51.
6. Cartwright MS, Shin HW, Passmore LV, et al. Ultrasonographic findings of the normal ulnar nerve in adults. Arch Phys Med Rehabil 2007;88:394-6.
7. Noto Y, Shiga K, Tsuji Y, et al. Nerve ultrasound depicts peripheral nerve enlargement in patients with genetically distinct Charcot-Marie-Tooth disease. J Neurol Neurosurg Psychiatry 2015;86:378-84.
8. European Society of Radiology (ESR). ESR statement on portable ultrasound devices. Insights Imaging 2019; 10:89.
9. Bathala L, Krishnam VN, Kumar HK, et al. Extensive sonographic ulnar nerve enlargement above the medial epicondyle is a characteristic sign in Hansen’s neuropathy. PLoS Neg] Trop Dis 2017;11:e0005766.
10. Shukla B, Verma R, Kumar V, et al. Pathological, ultrasonographic, and electrophysiological characterization of clinically diagnosed cases of pure neuritic leprosy. J Peripher Nerv Syst 2020;25:191-203
11. Reddy M, Pidaparthi L, Tourani V, et al. High-resolution ultrasound features of greater auricular nerve in leprosy. Postgrad Med J 2020;96:443.
12. Goedee HS, vanderPol WL, van Asseldark JH, et al. Diagnostic value of sonography in treatment-naive chronic inflammatory neuropathies. Neurology 2017;88:143-51
13. Won S J, Kim B-J, Park KS, et al. Measurement of cross-sectional area of cervical roots and brachial plexus trunks. Muscle Nerve 2012;46:711-6.